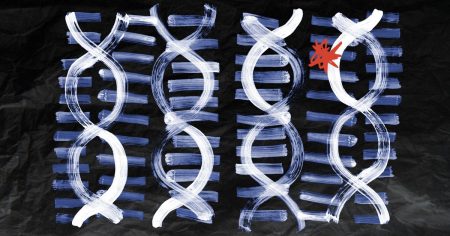
New research from the Francis Crick Institute in London has identified a genetic mechanism linked to the development of inflammatory bowel disease (IBD) and other autoimmune or inflammatory conditions. This discovery could potentially lead to the identification of drugs that could be used to treat these conditions. Scientists found a section of DNA that enhances the production of proteins in nearby genes, specifically in macrophages, an immune cell involved in IBD. This enhancement increased the activity of a gene called ETS2, which plays a crucial role in inflammatory functions in macrophages, contributing to tissue damage in IBD.
Though there are currently no drugs that directly target ETS2, the researchers found that MEK inhibitors, drugs used to treat cancer, could reduce inflammation in macrophages and gut samples from patients with IBD. This finding could pave the way for the development of new drugs and drug targets for treating IBD, a condition that affects an estimated 6 million people worldwide. The root cause of IBD is not fully understood, but genetics, diet, and gut microbiota have been suggested to play a role in its development. Further studies are needed to confirm the effectiveness of the identified medications in patients with IBD.
The complexity of IBD and other autoimmune diseases has posed challenges in developing effective treatments, with only a small percentage of drugs entering clinical development ultimately receiving approval for treatment. The recent focus on genetic pathways in disease development, such as the one identified in this research, may help address this issue. By connecting specific genetic variants to the regulation of a gene like ETS2, researchers have made significant advances in understanding the mechanisms that contribute to diseases like IBD. These findings have the potential to lead to more targeted and effective treatments with fewer side effects.
Experts emphasize the importance of further studies to validate the findings of this research, as experiments were primarily conducted in controlled lab settings. A broader test of the identified drug targets and pathways in living organisms could provide a more comprehensive understanding of their effects. While the ETS2 gene pathway may be relevant for a subset of IBD patients, the research methods used in this study could be applied to other diseases where genetic variants have unknown mechanistic connections. This broader application of the research findings may enhance the ability to target autoimmune diseases more effectively.
The ability to target the ETS2 gene through the findings of this research has the potential to lead to new treatments for IBD and other autoimmune diseases by reducing inflammation and limiting side effects. However, the delicate nature of these diseases and their pathways in the body may present challenges in developing precise and effective therapies. Careful consideration and development are necessary to avoid unintended effects on other bodily functions while targeting ETS2. By expanding the application of these research findings, the potential to develop new treatments for autoimmune diseases, including IBD, could be greatly increased.
Overall, the research findings from the Francis Crick Institute represent significant advances in understanding the genetic mechanisms that contribute to inflammatory bowel disease and other autoimmune conditions. By linking specific genetic variants to the regulation of the ETS2 gene and its impact on inflammatory functions in macrophages, researchers have identified potential drug targets that could lead to more effective treatments. Further studies are needed to confirm the effectiveness of these medications in patients with IBD and other autoimmune conditions, but the research opens up new possibilities for targeted therapies and improved understanding of disease development mechanisms.