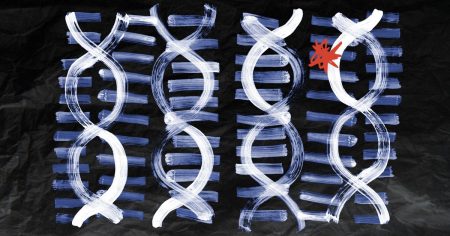
Endometriosis is a condition that causes cells similar to the uterus lining to grow elsewhere in the body, leading to inflammation, pain, and scar tissue. It is challenging to diagnose, with people waiting nearly 9 years from first reporting symptoms for a diagnosis. A recent study proposes that endometriosis can be diagnosed using a non-invasive stool sample to measure levels of a bacterial metabolite called 4-hydroxyindole (4HI), which is significantly lower in individuals with endometriosis than those without the condition. The researchers also demonstrated that 4HI reduced endometriosis initiation and progression in animal models, suggesting that it could be a potential treatment for the condition.
Endometriosis causes severe symptoms in up to 11% of women of reproductive age, with pain being the most common symptom. Other symptoms include long-term lower back and pelvic pain, heavy menstrual bleeding, bowel and urinary issues, blood in the stool or urine, nausea and vomiting, fatigue, pain during sex, spotting between periods, and difficulty conceiving. On average, people wait almost 9 years for a diagnosis, highlighting the need for improved diagnostic tools for endometriosis. The study suggesting the use of a stool sample to measure 4HI levels as a diagnostic tool has the potential to revolutionize the diagnosis of endometriosis, providing a simple and non-invasive method for identifying the condition.
Various studies have shown that individuals with endometriosis have a less diverse gut microbiome compared to those without the condition. The recent study analyzed stool samples from 18 women with confirmed endometriosis and 37 controls, identifying 371 metabolites, of which 61 differed between the two groups. Significantly, the metabolite 4HI was found to be reduced in stool samples of women with endometriosis, potentially due to alterations in gut microbiota. This distinct stool metabolite signature in those with endometriosis was similar to signatures seen in gut disorders like ulcerative colitis and Crohn’s disease, prompting further investigation into potential links between these conditions.
The potential connection between endometriosis and gut disorders such as IBD raises questions about common symptoms and overlaps between the conditions. The study’s findings suggest the possibility of utilizing a non-invasive stool test to diagnose endometriosis based on differences in stool metabolites between healthy individuals and those with the condition. The researchers are working on developing this diagnostic test, which is expected to take 2-5 years to make available for clinical use. Additionally, investigations into the administration of 4HI in animal models showed promising results in preventing inflammation and pain associated with endometriosis, raising the possibility of 4HI as a potential treatment for the condition.
While the study findings are promising, there is a need for further research to validate the diagnostic potential of the stool test and the efficacy of 4HI as a treatment for endometriosis. The small cohort size of the study necessitates larger-scale trials to confirm the results and assess the safety and effectiveness of potential treatments. However, the development of a non-invasive diagnostic tool and the identification of gut microbiota and metabolites as central to endometriosis pathogenesis offer new avenues for understanding and combating the disease. The study marks a significant step forward in improving the diagnosis and treatment of endometriosis, potentially benefiting women who suffer from this often-debilitating condition.