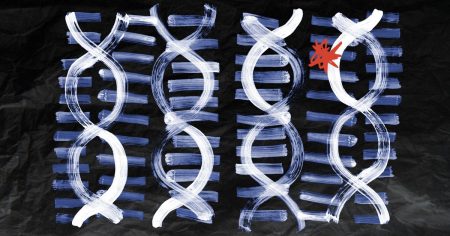
A recent study from the University of California, San Francisco, has potentially found a method for easier, earlier diagnosis of multiple sclerosis (MS). MS is a neurological disorder that affects almost three times as many women as men and is estimated to affect around 2.8 million people worldwide. Diagnosis of MS typically relies on a range of tests, including MRI scans, lumbar puncture, and evoked potential tests. However, researchers have identified a distinctive set of antibodies in the blood of people who later developed MS, which could potentially lead to a simpler, earlier blood test for the disease.
The study involved analyzing samples from 500 participants, including those who had developed MS and controls who did not have the disease. They found that levels of neurofilament light chain, a marker of nerve cell damage, were higher in those who later received an MS diagnosis many years before their first symptom flare-up. The researchers also detected a distinct pattern of autoantibodies in the blood of those who later developed MS, which they termed an ‘immunogenic cluster’. This signature was not seen in control participants, indicating its potential as a biomarker for MS.
The autoantibody signature identified in the study could have clinical potential for early diagnosis of MS, potentially allowing for earlier treatment initiation. The researchers suggest that an autoantibody serology test against the identified peptides could be used in a surveillance setting for patients at high risk of developing MS. Further research is needed to confirm the findings and explore potential uses of the autoantibody signature, such as predicting disease severity and explaining variability in the course of MS.
While early diagnosis could help many people with MS avoid severe symptoms, it may not benefit those with progressive MS who have limited treatment options. Caitlin Astbury, research communications manager at the MS Society in the UK, emphasized the need for new treatments for all individuals living with MS, in addition to early diagnosis. Living with MS can be debilitating, exhausting, and unpredictable, and early treatment is essential for improving outcomes and quality of life for those affected by the disease.
Overall, the study’s findings represent a significant step towards developing a simpler and earlier method for diagnosing MS. By detecting a unique set of antibodies in the blood of individuals who later develop the disease, researchers may be able to identify MS at an earlier stage, allowing for timely intervention and improved outcomes. Further research and validation of these findings are needed to fully understand the clinical implications and potential uses of the autoantibody signature for MS diagnosis and management.