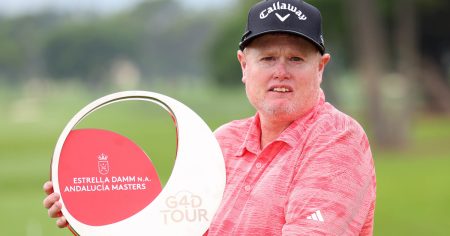
A woman with Type 1 diabetes underwent a groundbreaking stem-cell therapy using her own cells, resulting in her not needing insulin injections 75 days after the procedure. More people have since been enrolled in this trial, with promising results. The stem-cell derived islet cells successfully engrafted inside the woman’s abdomen, allowing her to produce her own insulin. Researchers in China are continuing to follow up with these patients in the ongoing trial, with a focus on a long-term follow-up of at least 2 years to assess the efficacy of the treatment.
The case study involved taking fat cells from a woman with Type 1 diabetes and converting them into pluripotent stem cells, which were then used to create islet cells that produce insulin. By injecting these induced islet cells into the patient, researchers observed successful engraftment and growth of vasculature, leading to the woman no longer needing insulin injections. Before the procedure, she only reached her target glycemic range 43.18% of the time, but four months later, this increased dramatically to 96.2% of the time. Her glycated hemoglobin levels also indicated a systemic glucose level at a non-diabetic level, showing the effectiveness of the treatment in maintaining blood sugar levels.
Other stem-cell-based therapies for both Type 1 and Type 2 diabetes are also in development and have shown promising results in clinical trials. Results from a phase 1/2 clinical trial on stem-cell derived Type 1 diabetes treatments showed positive outcomes for participants, including the successful introduction of insulin-producing islet cells. The trial, which began with 12 participants, expanded to include a total of 37 individuals. Researchers are focusing on developing immunomodulatory strategies and enhancing the clinical manufacturing process to make stem-cell treatments more efficient and cost-effective for a larger patient population.
The success of these stem-cell therapies in treating diabetes has garnered attention from researchers in the field, who are impressed by the results achieved in patients. The use of a patient’s own cells in the treatment process eliminates concerns about organ rejection and reduces the need for anti-rejection medications. While the results are encouraging, challenges still exist in making stem-cell treatments widely accessible to more patients with diabetes. Researchers are working on expanding and accelerating the process, ensuring the absence of unwanted or off-target cells, and developing efficient manufacturing techniques to advance stem-cell therapies for diabetes.
Despite the remarkable progress in stem-cell therapies for diabetes, researchers acknowledge the need for further advancements and improvements in the field. Challenges such as developing appropriate immunomodulatory strategies and ensuring cost-effective clinical manufacturing of stem-cell derived islets remain to be addressed. Collaborative efforts among research teams, healthcare professionals, and regulatory authorities are essential to overcome these challenges and extend the benefits of stem-cell treatments to a larger population of patients with diabetes. Continued research and innovation in the field of stem-cell therapy hold promise for revolutionizing diabetes treatment and improving the quality of life for individuals with this chronic condition.