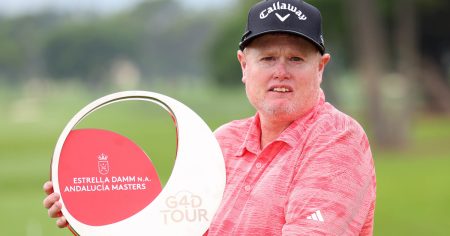
Older adults who have experienced a traumatic injury as a result of falling are more than 20 percent likely to later receive a diagnosis of Alzheimer’s disease or another related dementia, according to a new study published in JAMA Network Open. The retrospective cohort study conducted by researchers at Brigham and Women’s Hospital examined data from over 2 million older adults who had sustained a traumatic injury, with more than 10 percent of them later receiving a dementia diagnosis in the year following their fall. The average age of patients who experienced a fall was 78, and more women fell than men.
Some types of dementia, such as Alzheimer’s disease, result from the progressive death of brain cells and neurons over time. Head injuries can contribute to dementia through direct damage to cells. A loss of motor skills is part of the progression of Alzheimer’s disease, with people experiencing difficulty with balance, coordination, and orientation. The study’s senior author, Molly Jarman, emphasized that the connection between falling and cognitive decline can be a “two-way street,” as falls can also be a result of cognitive impairment.
The study’s first author, Alexander Ordoobadi, explained that the results do not provide a direct association between falls and dementia. Some patients may have had mild cognitive impairment at the time of the fall and later progressed to dementia, while others may have had undiagnosed dementia prior to the fall. Ordoobadi stressed the importance of cognitive screening for all older adults who are hospitalized as a result of a fall to aid in the early diagnosis of dementia.
Neurologist Clifford Segil mentioned that certain types of dementia, such as Lewy body dementia or Parkinson’s dementia, may increase the risk of falls. He highlighted the challenge of determining how a ground-level fall could worsen dementia, suggesting that certain brain injuries, such as subdural hematomas, could impact cognitive function. Segil also noted that age-related conditions like heart disease, diabetes, and Parkinson’s disease can contribute to falls, which can be linked to the development of dementia.
Ordoobadi emphasized that declines in cognition can affect motor skills, with mild cognitive impairment serving as a precursor condition to more serious forms of dementia. Walking requires substantial cognitive capacity to coordinate movements and maintain balance, and impairments in motor domains may precede the formal diagnosis of dementia. Segil supported the idea of advising patients who experience ground-level falls to undergo cognitive screening, as frequent falls can indicate a need for early detection and management of cognitive decline.
Both researchers emphasized the importance of recognizing the potential connection between falls and dementia in older adults, as well as the need for cognitive screening to identify cognitive impairment early on. Understanding the complex relationship between falls, cognitive decline, and dementia can help healthcare providers provide better care and support for older adults at risk. More research is needed to further investigate the mechanisms underlying this association and to develop effective strategies for preventing and managing falls and dementia in older populations.