The rise in the number of hip and knee replacements is projected to increase dramatically over the next few decades, with procedures representing the highest surgical expenditure for Medicare. The introduction of the bundled payment model symbolized a shift towards corporatization and mass scaling of joint replacements under the guise of “value-based care.” This has led to a High-Volume Joint Replacement Society where patients are orphaned by insurance plans and health systems, leaving surgeons to navigate the complex healthcare landscape.
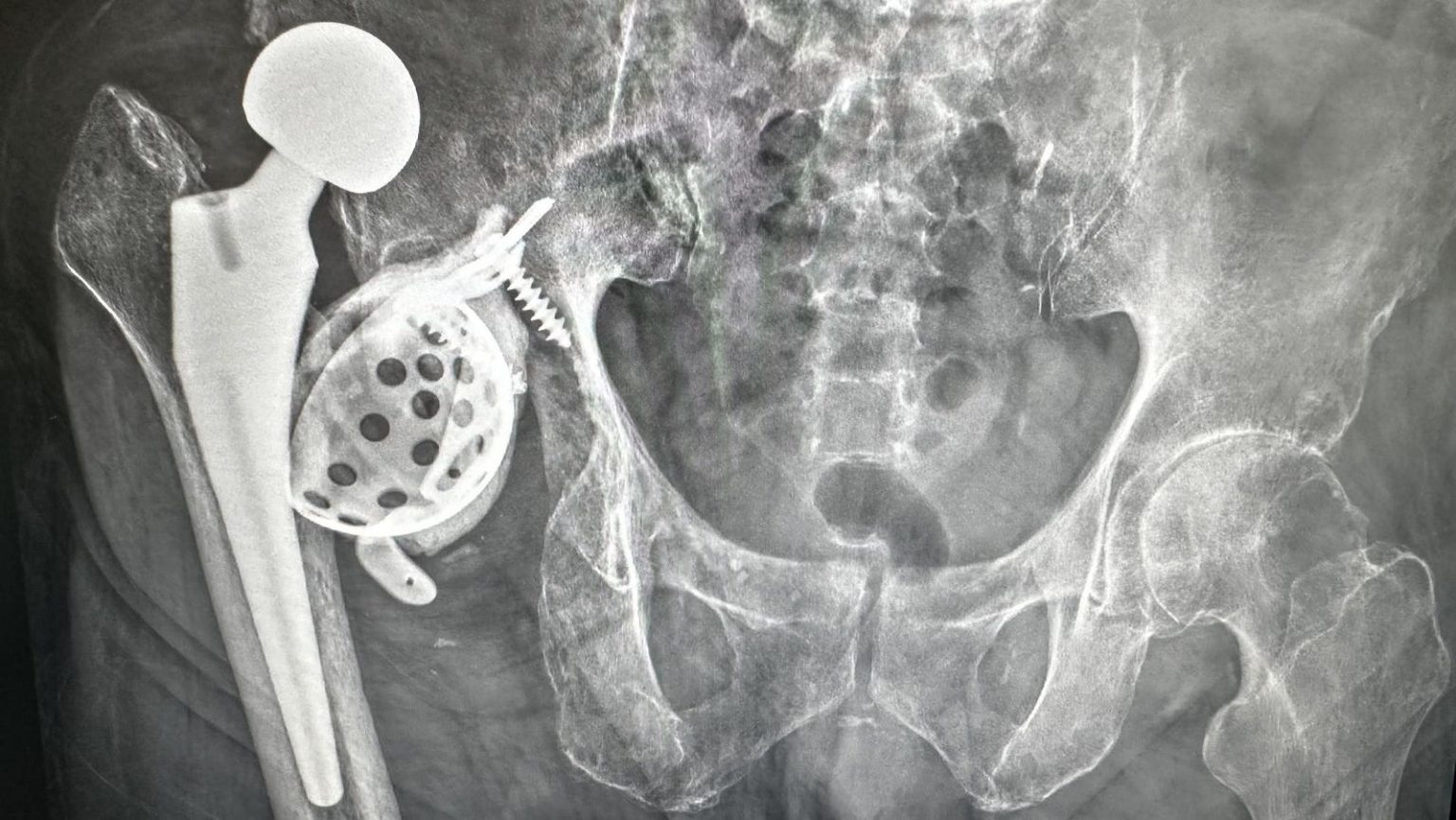
The societal perception of joint replacements as a quick fix for pain has overshadowed the potential long-term complications and risks associated with the surgery. Failed joint replacements can result in various issues such as infection, instability, loosening, wear, or fracture, with revision surgeries posing greater challenges and risks. The current infrastructure disincentivizes hospitals and surgeons from caring for patients with failed joint replacements, leading to significant resource allocation and higher costs.
Surgeons managing failed joint replacements face increased complexity, longer procedures, and higher mental and physical burdens compared to first-time surgeries. The financial loss for surgeons and healthcare systems when caring for patients with failed joints is substantial, creating challenges for those dedicated to providing comprehensive care for these complex patients. The lack of proper incentives and support for surgeons tackling these challenging cases needs to be addressed in order to improve patient outcomes and surgeon satisfaction.
The discussion around success of joint replacements needs to shift from focusing solely on how long the replacement lasts to considering the lifetime failure risk associated with the surgery. Younger patients undergoing joint replacements carry the highest lifetime risk of failure, which may influence decisions regarding the timing of the operation. While most patients do well after joint replacements, the potential for failure and complications should be openly discussed and factored into decision-making processes for both patients and surgeons.
The emphasis on commoditizing joint replacements through mass scaling and profit-driven healthcare systems poses a significant challenge for the future of joint replacement surgeries. Efforts to prevent complications, establish preferred centers for managing failed joint replacements, and prioritize joint-preserving strategies when possible are essential steps in combating the potential crisis of failed joint replacements at a population level. Addressing the systemic issues and prioritizing patient outcomes over profits is crucial for ensuring the long-term success and sustainability of joint replacement surgeries.