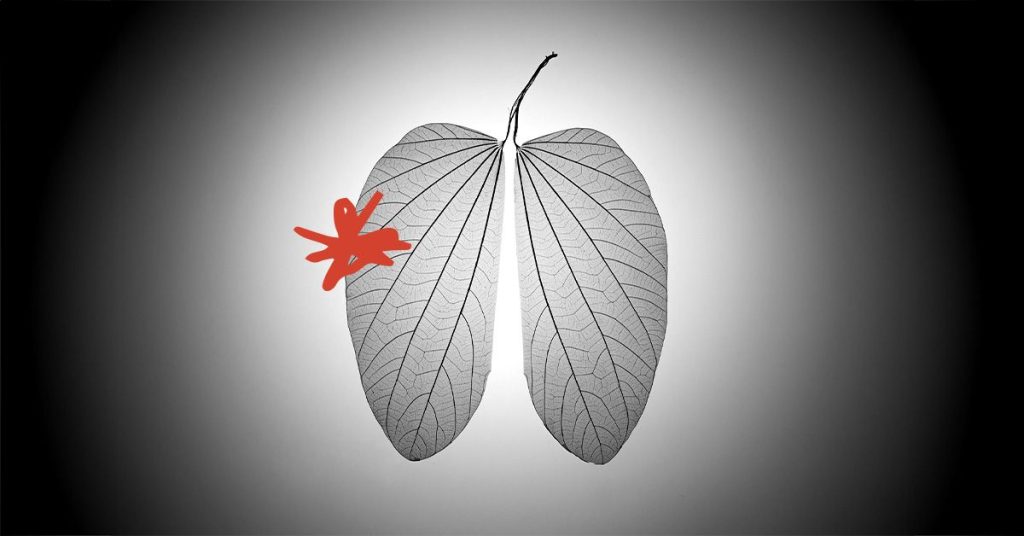
Researchers have found that individuals who have never smoked may be less responsive to standard treatment for non-small cell lung cancer (NSCLC), with a combination of two genetic mutations potentially making cancer cells more resistant to therapy. There is a need for new diagnostic tests and targeted therapies to address these treatment-resistant cases. Between 10% to 20% of people who develop lung cancer are non-smokers, and the reasons behind this remain unclear, with factors such as genetics, environment, and lifestyle all potentially playing a role. Lung cancer in non-smokers is the fifth leading cause of death worldwide, underscoring the importance of understanding and addressing these cases.
Non-smokers with NSCLC can exhibit resistance to targeted treatment, with 10% to 15% of patients not responding well to standard therapies. A recent study found that a mutation in the EGFR gene, often present in non-smokers with NSCLC, when combined with a mutation in the p53 gene, led to the development of drug-resistant tumors. These findings shed light on why some patients with EGFR mutations have poor survival outcomes, as tumors with both mutations were more likely to grow after treatment, resulting in chromosomal instability and increased resistance to therapy. There is currently no test available to detect this dangerous genome doubling, but work is underway to develop such a diagnostic tool.
Researchers are focusing on developing targeted treatment strategies for NSCLC patients with these specific mutations. By identifying patients with both EGFR and p53 mutations whose tumors display genome doubling, it may be possible to treat them more effectively through a more selective approach. Combination therapies involving targeted treatments and other therapies are emerging as potential interventions to prevent the development of drug resistance. However, it is important to carefully consider the balance between treatment efficacy and toxicity in these combination approaches to ensure the best outcomes for patients.
Non-small cell lung cancer experts are emphasizing the importance of tailoring new therapies to address cases where standard treatments are ineffective. Genetic testing can help identify new mutations in tumors that may be causing resistance to targeted therapies, allowing for the selection of interventions that can overcome these resistance mechanisms. Experimental drugs are being developed to target specific resistance mechanisms, providing new avenues for treatment in cases where established therapies are no longer effective. This personalized approach to treatment could lead to better outcomes for patients with NSCLC, particularly in cases where resistance to standard therapies is a challenge.
The proportion of lung cancer cases in people who have never smoked has been increasing in recent years, especially among women and younger age groups. The reasons behind this increase in non-smoking-related lung cancer cases remain unclear, highlighting the need for further research to better understand the underlying factors contributing to these cases. Developing targeted therapies and diagnostic tools to address the unique challenges faced by non-smokers with NSCLC is crucial to improving outcomes and providing more effective treatment options for these patients. By investigating the genetic mechanisms driving drug resistance in non-smokers with NSCLC, researchers hope to develop innovative treatment strategies that can overcome these challenges and improve survival rates for this population.