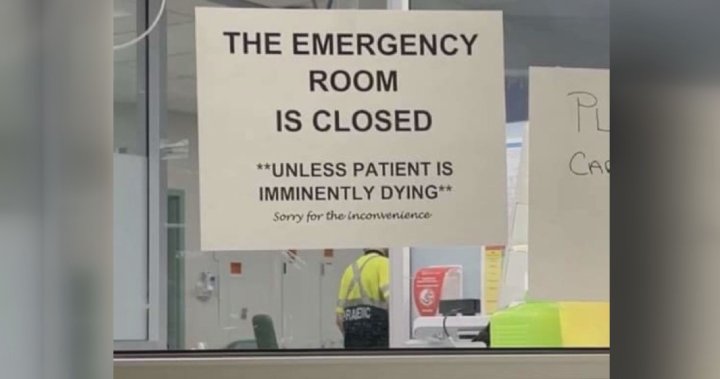
Residents in several communities in British Columbia face the dreaded daily wait at four o’clock to learn if their local emergency department will be closed temporarily. This issue is particularly pressing for those who rely on the Caribou Memorial Hospital in Williams Lake, which has experienced 10 closures in July alone, with most occurring on weekends. The mayor of Williams Lake emphasizes the importance of the hospital as a regional facility serving tens of thousands of people. Similarly, other communities within Interior Health, such as Merritt, Lilooet, Oliver, and Creston, have also faced frequent temporary closures of their emergency departments, totaling 62 since the beginning of the year. The closure of the local emergency room in Dawson Creek due to nursing coverage challenges further highlights the severity of the issue.
Mayors from affected B.C. communities have expressed their frustration with the ongoing closures. Merritt Mayor Michael Goetz, for example, has threatened to send the province an $84,000 bill for emergency department interruptions that put a strain on the fire department last year. Cariboo-Chilcotin MLA Lorne Doerkson has organized a community rally to demonstrate widespread concern over the closures. The closures are primarily attributed to staffing shortages among physicians and nurses, compounded by issues related to vacations, absences, and the continuing effects of the pandemic. Health Minister Adrian Dix acknowledges that staffing challenges have contributed to the problem, but emphasizes the efforts being made to recruit and retain healthcare professionals in rural communities by providing incentives and offering alternative payment models.
While some communities such as Clearwater have successfully avoided diversion for extended periods by implementing strategies like providing additional housing for healthcare workers, the ongoing closures continue to impact various sectors of the healthcare system. Ambulance Paramedics of BC president Jason Jackson highlights the added stress on paramedics due to longer response and transportation times, as well as concerns about the impact on patient care during critical health emergencies. The province has added 19 additional ambulance units in affected communities, but Jackson stresses the need for a long-term solution to address the overall staffing challenges faced by the healthcare system.
Local leaders like Mayor Rathor and MLA Doerkson are calling for further action to address the ongoing emergency department closures. Rathor has requested an internal audit from Interior Health to address the diversion issue and proposes expanding nursing programs to increase the number of healthcare professionals in the community. Doerkson advocates for improved communication from the health region with the community and the involvement of an independent agency to conduct audits or reviews to prevent future closures. As the community continues to grapple with the impact of these closures on healthcare access and patient outcomes, urgent measures are needed to address the underlying staffing challenges and ensure the well-being of residents in these communities.
In response to the growing concerns over emergency department closures, Health Minister Adrian Dix acknowledges the staffing challenges and emphasizes the province’s efforts to recruit and retain healthcare professionals in rural communities. Dix points to initiatives such as hiring additional nurses and moving away from fee-for-service payment models for doctors as steps towards addressing the staffing shortages. While some communities have successfully avoided diversions through initiatives like providing housing for healthcare workers, the ongoing closures continue to affect various sectors of the healthcare system. Urgent action is needed to address the underlying staffing challenges and prevent further disruptions in emergency healthcare services.