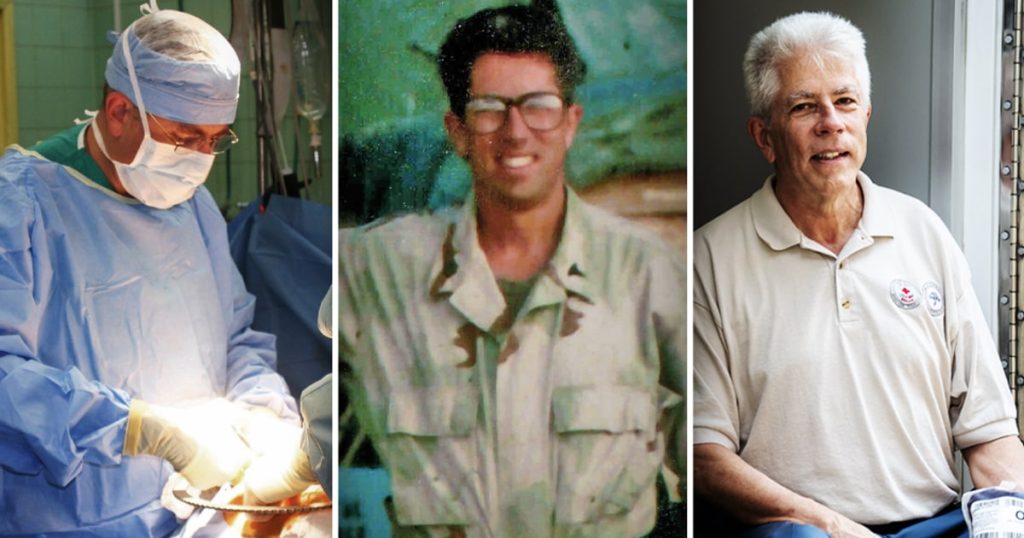
In 2016, there were no emergency medical service agencies offering blood transfusions during rescue missions in the United States. However, there are now 152 agencies across 23 states that provide this critical treatment. Dr. Jeffrey Kerby, a former Air Force trauma surgeon, and other doctors are leading the charge to expand the availability of blood transfusions in rescue vehicles. They believe that this treatment could save the lives of at least 40,000 to 60,000 people if insurance providers start reimbursing for it.
Trauma is the leading cause of death in the U.S. for people aged 1 to 45, and studies show that receiving blood prior to arrival at a hospital significantly improves survival rates. Despite these statistics, most ambulances and rescue helicopters in the U.S. administer crystalloid, which can be ineffective and even harmful for bleeding patients. The value of whole blood transfusions has been recognized by former trauma surgeons with battlefield experience, who now advocate for its availability in communities across the country.
The journey towards integrating blood transfusions into rescue vehicles began with Dr. Donald Jenkins, an Air Force trauma surgeon stationed on a desert island off the coast of Oman in 2001. Jenkins was forced to provide care for wounded soldiers without prior training in whole blood transfusions. His use of whole blood in treating these casualties had “magical” results, leading him to champion the integration of blood into rescue services in San Antonio. Through a unique reimbursement system and collaboration with blood donation centers, San Antonio has successfully implemented prehospital blood transfusions, saving an estimated 2,000 lives.
One example of the impact of prehospital blood transfusions is the case of a 12-year-old girl named Mayah Zamora, who was critically injured in a school shooting in 2022. Mayah received a blood transfusion during the helicopter ride to the hospital, which played a crucial role in saving her life. Another case involves a 6-year-old Florida girl named Izzy Niemczyk, who experienced a life-threatening bleed following a tonsillectomy. Thanks to the newly implemented prehospital blood transfusion program in Palm Beach County, Izzy received a transfusion in the ambulance, leading to her rapid recovery and survival.
The availability of whole blood in rescue vehicles has been a transformative development in emergency medical care, with the potential to save thousands of lives across the country. However, challenges remain in expanding this initiative, including the need for insurance providers to reimburse for blood transfusions in rescue settings. Despite these obstacles, the dedication and perseverance of medical professionals like Dr. Jeffrey Kerby and Dr. Donald Jenkins continue to drive the push for widespread access to prehospital blood transfusions as a crucial intervention in saving lives.
Overall, the integration of blood transfusions into prehospital emergency care represents a significant advancement in trauma treatment in the U.S. With the support of medical professionals, local communities, and policymakers, the initiative to provide blood transfusions in rescue vehicles has the potential to save countless lives and improve outcomes for individuals facing life-threatening injuries. Through continued advocacy and collaboration, the vision of widespread access to prehospital blood transfusions as a standard of care in emergency medicine may soon become a reality.