Asthma, a chronic lung disease that affects millions of people worldwide, has no cure despite the availability of treatments to manage symptoms. However, recent research has identified a potential unexpected cause of asthma that could lead to new ways to combat the disease. Scientists have discovered a glitch in the mechanical process that drives the turnover of epithelial cells lining the lungs, known as cell extrusion. This physical force may be responsible for chronic asthma attacks, and a better understanding could potentially lead to more effective treatments for the disease.
Cell extrusion is the process by which epithelial lung cells replicate, causing overcrowding and increased pressure. Weaker cells are then ejected from the layer, maintaining a healthy epithelial lining in the airways. Previous research has hinted at the involvement of this process in asthma, but researchers have traditionally focused on other triggers of the disease. With asthma affecting a significant number of people globally and often contributing to severe health issues, understanding the role of cell extrusion in the development of the disease could be crucial.
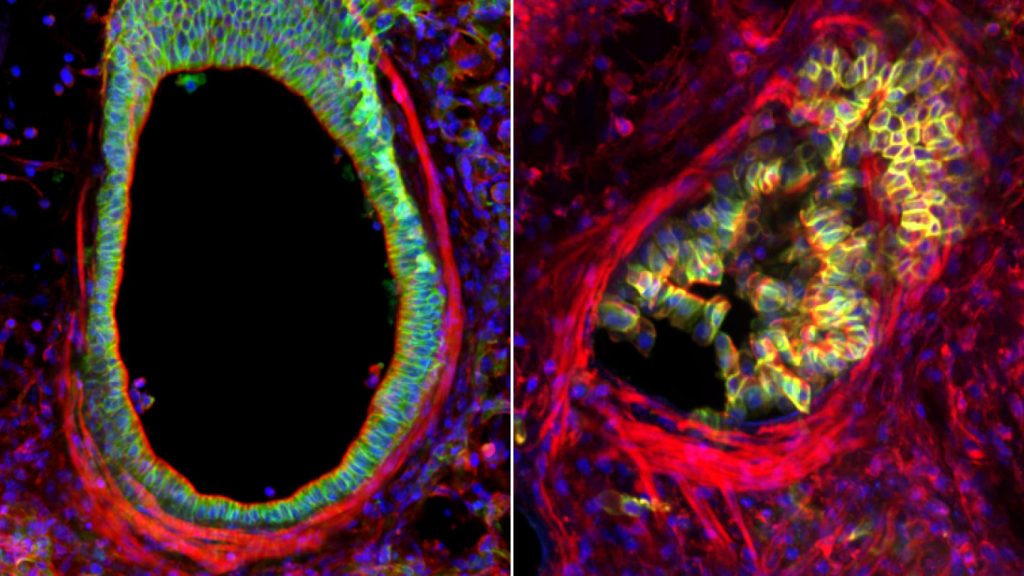
A study conducted by cell biologist Jody Rosenblatt and her team explored the link between asthma and cell extrusion. Through experiments on living mouse lung cells and human airway samples, they discovered that asthma attacks could lead to severe cell extrusion, mucus buildup, and damage in the airways. The pressure from asthma attacks can trigger a vicious cycle of cell death, damage, and future attacks, highlighting the potential impact of this mechanical process on disease progression.
Treatment with traditional asthma drugs, such as albuterol, was found to ease airway constriction during asthma attacks but did not reverse the resulting damage. Relaxing the airways with albuterol may create gaps in the epithelial lining, making individuals more susceptible to allergens and irritants. This could explain why some people with asthma report feeling worse over time despite medication, as the underlying damage persists.
Further experiments involving the inhibition of piezo1, a protein that senses mechanical pressure in epithelial cells, showed promising results. Blocking these cell receptors reduced excess cell extrusion, inflammation, and mucus production, suggesting a potential avenue for preventing asthma-related damage. Continued research is needed to explore the clinical applications of these findings in both animal models and human patients.
Overall, this research provides a valuable insight into the role of mechanical forces in the development and progression of asthma. Understanding how physical processes impact disease pathology could lead to novel treatments that target the underlying cause of asthma rather than just managing symptoms. This work represents a step towards more personalized and effective therapeutic approaches for individuals living with asthma.